Anaesthesia Free Dentistry For Dogs and Cats
Anaesthesia free dentistry for dogs and cats is being promoted as the new wave of safe and appropriate dental care for our pets.
But is it really?
The process of anaesthesia free dentistry requires a dog to be physically restrained, usually on its back, and have visible tartar picked off.
Because these procedures are performed by people with no formal training i.e., not veterinarians, it is illegal for them to check for abnormalities below the gum line or diagnose.
That’s assuming that these people have the knowledge to recognise a problem in the first instance.
In this article, we discuss why many welfare advocates and veterinarians believe that anaesthesia free dentals are a poor substitute for dental examinations performed by veterinarians under general anaesthesia.
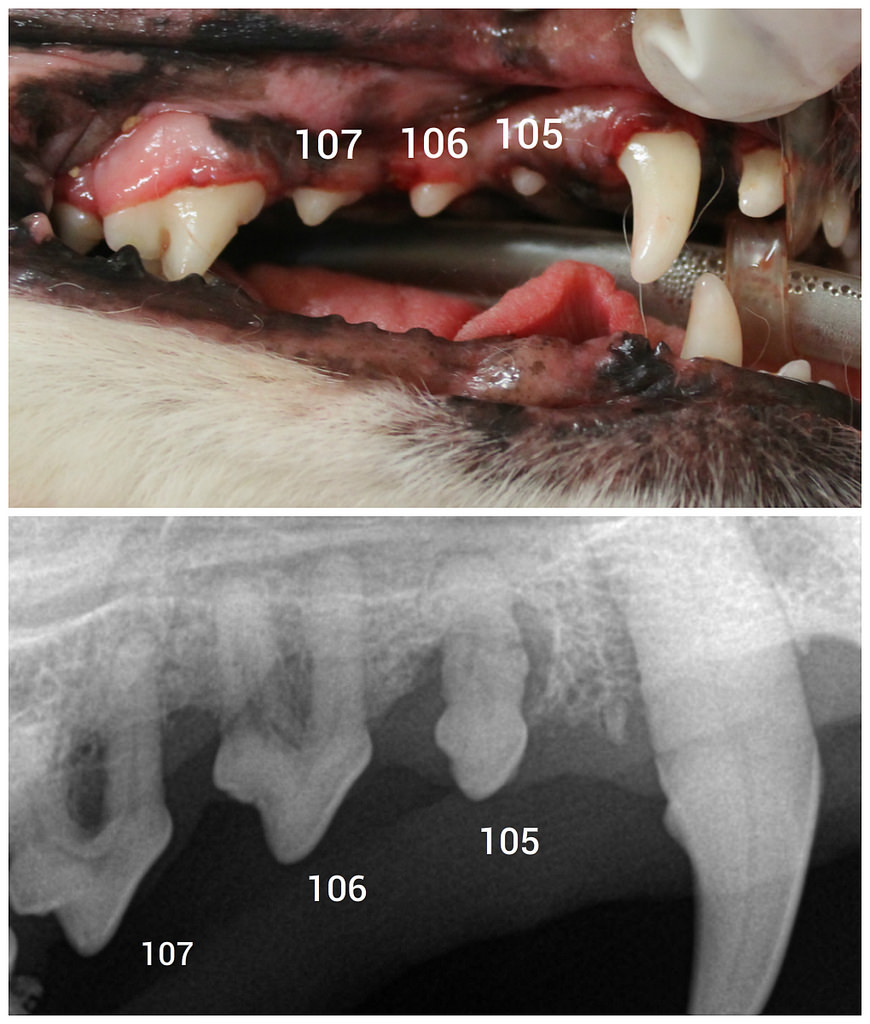
Only radiographs could identify the periodontal disease and bone loss affecting this dog’s teeth. We perform dental charting and did not find any pocketing or mobility associated with 105-107, yet all three needed to be extracted due to >50% bone loss affecting each. Photo credit Mariposa Veterinary Wellness Centre
Mel Asked Dr Leigh The Following Question:
My kitties are due for a dental check up, I’m considering having a anaesthesia free dentistry procedure performed. Can you please tell me the pros and cons of anaesthesia free dentistry for dogs and cats? I’m also concerned about anaesthetic risk. Do I need to be?
Dr Leigh Replies
Mel you aren’t alone! These are questions I am asked time and time again, so let’s take a moment to walk through what happens when a registered vet performs a dental exam and scale and polish treatment in comparison to when a layperson removes tartar from your pet’s mouth.
The Anaesthesia Free Process
Imagine lying back in your mother’s lap, she’s holding open your mouth and scraping your teeth with a sharp metal tool.
“Ouch” she’s hit the edge of your gum, you wiggle and squirm and she pins you still.
Ewwwwww that familiar iron taste of blood fills your mouth.
You want to close your mouth and swallow, “mmmaaaaaaa” your mother relaxes her grip on you and you close your mouth and ask for a glass of water to rinse the horrible blood taste from your mouth.
Lying back again, your mother moves the tool over your teeth scraping away the tartar, and then much to your surprise, you are in agony.
“Whoa” the tool has scraped across an area of the tooth that lacks enamel, it’s super sensitive.
That’s it….no more….you’ve had enough and you aren’t going to sit around for this anymore.
That, my friends, is exactly what is going on for your dog or cat when you subject them to anaesthesia free dentistry.
Except they cannot tell you to stop. They can’t say “I need to swallow”.
Anaesthesia Free Dentistry Subjects Your Dog To Pain, Fear And Anxiety
One of the main cons of anaesthesia free dentistry in dogs and cats is the fear and anxiety that it can cause.
We can’t explain to our pets what is happening.
All they experience when they are forced to lie back and open their mouth, is discomfort, pain and anxiety.
Every time a metal tool goes close to the gum line there is potential for it to cut that gum and touch exposed dentine.
I have exposed dentine due to enamel hypoplasia, and I can tell you I struggle at the dentist.
It is the most painful experience I’ve encountered. I want to get out of that chair so fast.
Our pets are no different.
Consider this, how can someone hold an animal on its back and assess its teeth and clean away tartar without that animal being scared?
How can each tooth be individually examined and probed?
How can the gumline around each tooth be probed?
The answer is they can’t be.
And here lies the problem.
This process concentrates on removing tartar from the easily accessible crown of the tooth only.
It is a cosmetic option with no examination of individual teeth, the gum line or the underlying bone and root structures.
It is impossible to reach some teeth in some dogs as the dog just isn’t relaxed enough to open its mouth wide enough for you to have a probe around the tooth.
A Complete Oral Exam Cannot Be Performed With An Awake Animal
Another major concern vets have with anaesthesia free tartar removal is that there is no examination under the tongue, the very back of the mouth (pharynx), probing of tooth holes or gingival pockets, or taking radiographs.
It is impossible to assess the whole mouth properly in an awake dog.
Often, in dogs with periodontal disease (usually the older toy breeds), the amount of disease and inflammation is so great that the strength of the jaw bone is not enough to resist fracture.
As the jaw is manipulated it fractures, usually around the first molar tooth.
I have seen and heard of cases that have presented to a veterinarian with a broken jaw after an anaesthesia free cosmetic procedure.

1 Total loss of attachment 2 Gingival recession 3 Probing depth of periodontal pocket By Lesion (Own work) [CC BY-SA 3.0], via Wikimedia Commons
The following conditions are missed when you don’t use anaesthesia because it’s impossible in many situations not to cause pain, or to visualise the problem:
- gingival recession
- periodontal pockets and disease
- pulp exposure
- tooth and jaw fractures
- resorptive lesions
- dead teeth
- abscesses or infected teeth
- broken tooth roots
Unfortunately for our pets, this means that they continue to feel pain and discomfort as treatable conditions remain untreated.
You as the owner will likely need to spend more money getting the problems fixed at a later date by a veterinarian.
Some places are now offering anaesthesia free dog teeth cleaning that uses sedation! This is still inappropriate for the same reasons.
It is ILLEGAL for NON-VETS to sedate your pet. A veterinarian must be registered in your state to use anaesthesia, nerve blocks or sedation. If you suspect your animal has been sedated please alert your local veterinary board.
Why Vets Cannot Recommend
Tartar Removal Is Cosmetic Only
The teeth may look pearly white, and the breath may smell better, but there is no way of knowing what is happening below the gum line or within individual teeth.
The Process Is Stressful & Painful
The risk of ongoing behavioural issues related to the examination of your pet’s mouth is high.
The Process Is Expensive
There are no animal health benefits providing a false sense of security.
The cost of a GA Free tartar removal ranges from $250 to $450. Exactly the same as what many vets charge for a routine scale and polish under anaesthesia.
Why sacrifice appropriate care by veterinarians – experts in animal health?
The cost of a GA Free tartar removal ranges from $250 to $450. Exactly the same as what many vets charge for a routine scale and polish under anaesthesia. Why sacrifice appropriate care?
Is General Anaesthesia A Risk?
General anaesthesia is not risk-free, however, risks can be managed.
Before your dog (or cat) is placed under anaesthesia a full clinical exam is performed.
This includes not only assessing the mouth and teeth and advising you of what may be needed but also to check the other organ systems for abnormalities.
Depending on what is found on the examination, your vet may recommend a pre-anaesthetic blood screen. This is to ensure that we can adjust the anaesthesia to suit your animal the best.
Blood tests become more important as your animal ages or if they have any pre-existing medical conditions. Vets are looking for changes in liver and kidney function that may support a different type of anaesthesia protocol.
As Mel mentioned, the risk of anaesthesia is something that many people rightly have a concern about. We are lucky that in this day, our drugs are very safe and side effects are very minimal when compared with the old days. You may have heard the saying:
“There are no safe drugs only safe anaesthetists.”
However, just like humans, there is always a risk of death with a GA.
If your vet is concerned about an anaesthetic risk, it is possible that they don’t have the equipment and/or staff to monitor anaesthesia appropriately.
If this is a concern, you always have the option to ask your vet to refer you to another vet or a specialist who has the facilities to cope with advanced anaesthetic monitoring.
To minimise the anaesthetic risk your vet will:
- Suggest a pre-anaesthetic blood screen
- Use IV fluids during the procedure
- Use monitoring equipment like an ecg (or oesophageal stethoscope), pulse oximeter, non-invasive blood pressure monitoring and temperature gauge
- Ensure that the airway is protected by using an endotracheal tube
- Ensure that there is access to the blood stream i.e. a catheter is placed in a vein
If your pet has an existing condition such as a heart murmur or diabetes, special precautions are taken to ensure that your pet is kept safe.
The risk of your dog or cat falling ill from periodontal disease is higher than death from anaesthesia.
Anaesthetic risk is not an excuse to NOT perform a dental. Ask your vet for a referral to a specialist if you are concerned.
In fact, 70% of adult cats and 90% of dogs have periodontal disease.
Studies have shown that this can cause major problems with health and well being – just like in humans. To view studies click here.
Examination Of Teeth Under Anaesthesia
When your dog or cat is anaesthetised your vet will examine the whole mouth and pharynx.
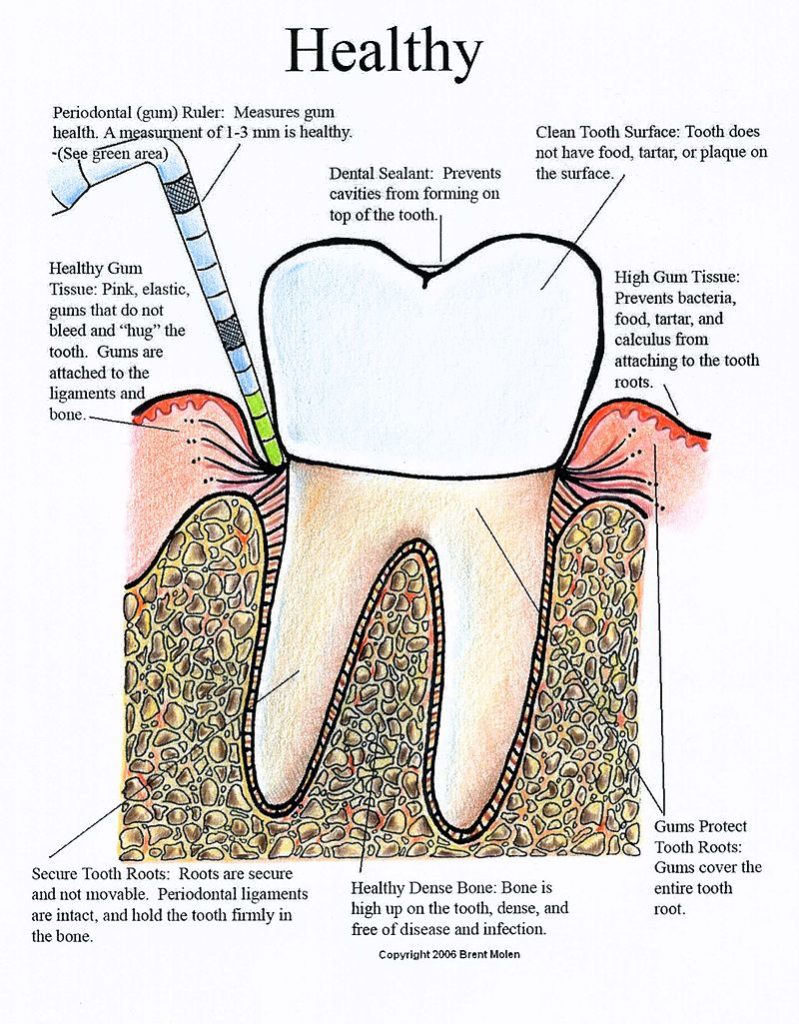
Take a look at this diagram to understand the anatomy.
The vet will be checking for:
- the number of teeth (there should be 42)- are there too many or are there any missing teeth?
- hair and food accumulation around teeth
- any sign of deformities such as a cleft palate
- any unusual lumps and bumps that may indicate a tumour or cyst
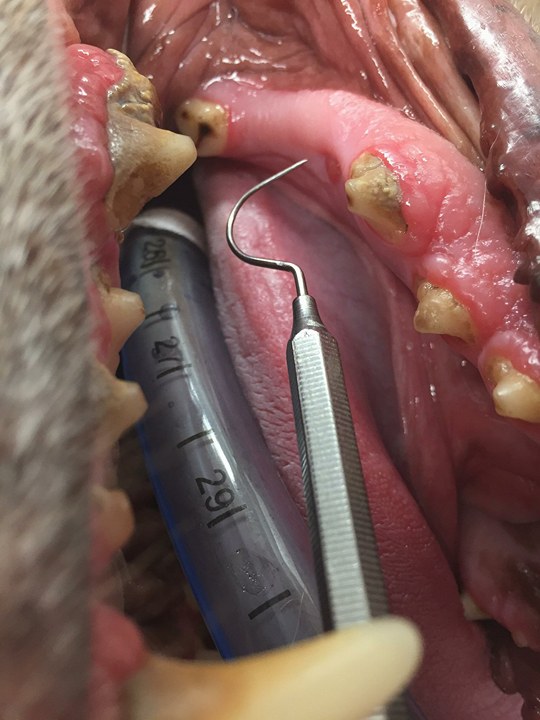
Next is the examination of the gingival sulcus.
The normal depth of the gingival sulcus in dogs is 0.5mm to 3mm while in cats it is 0.5mm.
When probing this area the vet is looking for an abnormal increase in depth of the sulcus.
Notes are made on whether the gingiva is swollen and oedematous ie. has gingivitis and whether there is any gingival recession that has led to root exposure.
Each tooth crown is thoroughly examined for signs of fracture, enamel hypoplasia and pulp exposure.
It can be amazing that what appears normal on a visual examination, can actually be a serious disease when you are able to view the mouth properly under general anaesthetic.
An example of this is in these pictures shared by Dr Aaron Forsayeth. Here we can see that a tooth is missing. It would be easy to ignore. However, because the dog is under anaesthesia we can take an xray and see that there is a tooth present. It just hasn’t erupted.
 In this view it appears that a tooth is missing.
In this view it appears that a tooth is missing.
 There is an indent where the tooth should be on a visual exam.
There is an indent where the tooth should be on a visual exam.
 On xray we can see that there is a tooth root present.
On xray we can see that there is a tooth root present.
Take a look at this video of Dr Aaron Forsayeth performing a dental exam on a dog under anaesthesia.
Note how thoroughly each tooth gingival pocket is examined, and imagine trying to do this in an awake dog.
How A Mouth Is Examined Under Anaesthesia
Are Xrays Of My Dog’s Teeth Necessary?
Once a full mouth examination has been performed, many vets will take radiographs of the mouth.
It is generally recommended to have xrays performed once a year.
Radiographs allow us to view disease under the gum line.

Col. Kenneth Boone, 375th Dental Squadron endodontist, prepares to take an initial X-ray of the tooth of Jack, a 375th Security Forces Squadron military working dog, prior to root canal surgery at the 375th Dental Squadron clinic April 21, 2011 at Scott Air Force Base, Ill. Jack, a bomb detection military working dog assigned to Scott, broke his tooth during patrol training. (U.S. Air Force photo/Staff Sgt. Brian J. Valencia)
Conditions that we can visualise on radiographs but may miss on clinical inspection include:
- Tooth root and bone resorption.
- Cysts
- Tumours
- Retained teeth
- Tooth crown, root and jaw fractures
- Abscesses
- Draining sinuses
- Periodontal disease
- Cups
- Foreign objects
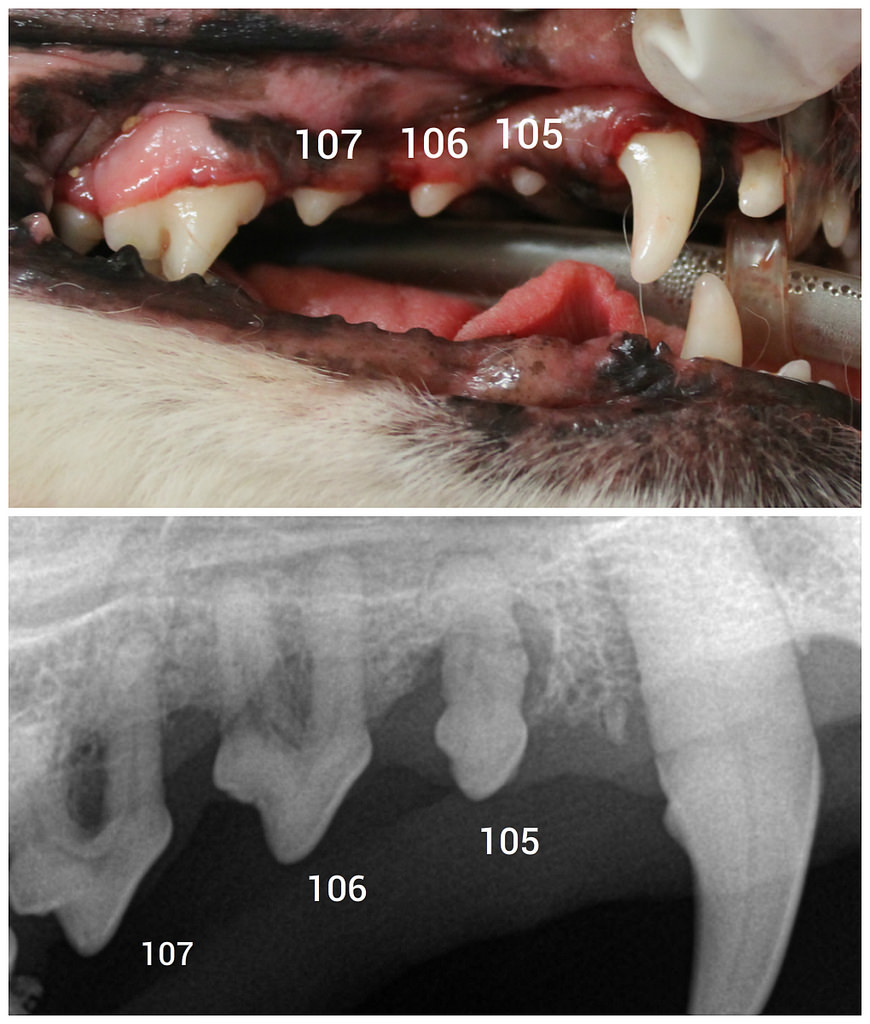 Only radiographs could identify the periodontal disease and bone loss affecting this dog’s teeth. We perform dental charting and did not find any pocketing or mobility associated with 105-107, yet all three needed to be extracted due to >50% bone loss affecting each. Photo credit Mariposa Veterinary Wellness Centre
Only radiographs could identify the periodontal disease and bone loss affecting this dog’s teeth. We perform dental charting and did not find any pocketing or mobility associated with 105-107, yet all three needed to be extracted due to >50% bone loss affecting each. Photo credit Mariposa Veterinary Wellness Centre
 This radiograph shows a dentigerous cyst next to the canine.
This radiograph shows a dentigerous cyst next to the canine.
 An example of bone resorption around tooth roots (Arrows).
An example of bone resorption around tooth roots (Arrows).
 Severe loss of bone density has lead to a fracture in this jaw.
Severe loss of bone density has lead to a fracture in this jaw.
Scaling And Polishing Dogs Teeth Under General Anaesthesia
If you haven’t watched the video above detailing how an examination of your dog’s (or cat’s) mouth is performed, go take a look now.
Scaling teeth can be performed with either a hand tool or an ultrasonic scaler.
Both are very sharp and if used incorrectly can damage the surface enamel of the tooth. If you slip you can cause severe lacerations to the lips, tongue or gums.
It takes a lot of pressure to use a hand tool.
In an awake dog, this would be very dangerous.
The most important part of the scaling process is removing tartar and plaque biofilm from under the gum line.
Remember, if this area under the gum line isn’t cleaned, scaled and polished appropriately then you are not preventing the development of periodontal disease (and wasting your hard-earned money).
Periodontal disease is what is going to cause systemic disease in your cats and dogs i.e. heart, kidney, liver disease.
There is a lot of water used in the process to flush away bacteria and chipped off tartar.
Animals aren’t very good at responding to commands such as rinse and spit, so anaesthesia is required.
The final aspect of cleaning the crown is polishing.
Polishing removes any small divots or grooves in the tooth enamel that scaling caused. It is an extremely important process as it discourages plaque and bacteria from adhering to the surface of the tooth.
In this video Dr Aaron Forsayeth demonstrates how scaling and polishing is performed.
Scaling and Polishing Dog Teeth
If My Pet Needs Extractions – How Will They Eat?
Before you gasp in horror, pets are not like humans. They don’t receive the same dental care that we give ourselves so extractions are common.
Remembering that over 70% of cats and 90% of dogs have periodontal disease, it should be no surprise when your vet tells you that your cat or dog needs a tooth or teeth extracted.
The process of extraction is sometimes straightforward ie. the tooth is removed with very little pressure due to extensive rot and disease.
Other times, it is a very involved process involving surgical flaps and specialised equipment.
One thing to note, removing teeth is not a fun job for your vet! It is hard work.
Your pet, however, will be so thankful. There are no worries about eating and they feel better.
Many clients note how their dog or cat seems to get a ‘new lease on life’.
Remembering that over 70% of cats and 90% of dogs have periodontal disease, it should be no surprise when your vet tells you that your cat or dog needs a tooth or teeth extracted.
Tooth Root Extraction In A Cat
Signs And Causes of Dental Disease In Dogs
Please check if your dog has any of these signs. If they do, please consult a veterinarian for a dental exam.
|
Signs And Causes of Dental Disease In Cats
Please check if your cat has any of these signs.
If they do, please consult a veterinarian for a dental exam.
Remember that cats hide pain very well, so even a small change in behaviour can be a sign of significant disease, whether in the mouth or in another body system.
|
The most important thing you can do as an owner of pets is to have your veterinarian examine and treat your pet’s teeth every 6 months.
Keep an eye out for our next article describing ways you can help keep your pet’s teeth healthy at home.
Do you want a weekly helping of Dr Leigh’s Vet Advice? Sign up for our weekly newsletter here.
I hope that answers your question Mel.
If anyone has any further questions, ask them below. Be sure to share this article with friends with dogs and cats. Let’s help all our cats and dogs live long, healthy lives.
You can listen to Dr Leigh discuss anaesthesia free dentistry for dogs and cats in this Facebook Live video.








Leave A Comment